Patient Information

Hip Dysplasia in Teenagers and Young Adults
What is Hip Dysplasia?
Developmental Dysplasia of the hip (DDH) is an umbrella term used to describe various bony abnormalities which result in poor containment of the ball of the hip (femoral head) within the hip socket (acetabulum).
It is a condition where the hip joint has not developed properly and this can affect; the shape of the bones, the orientation of the ball or socket, or all the above. Ultimately there is a mismatch in the fit of the ball into the hip socket, meaning that the femoral head is not held tightly in place and therefore increased movement (shearing) occurs. In very severe cases the ball can come out of the socket (dislocate).
Hip joint anatomy
The stability of the hip joint relies upon the following structures:
- The shape of the bones: The femoral head and the acetabulum
- Cartilage: Connective tissue covering the surface of the joint
- Labrum: Ring of cartilage, which sits around the rim of the hip socket
- Ligaments: Connect 2 bones together to provide further stability. There are four main hip ligaments:
• Ischiofemoral ligament
• Iliofemoral ligament
• Pubofemoral ligament
• Ligamentum Teres - The joint capsule: A strong and dense fibrous sac that surrounds the hip joint
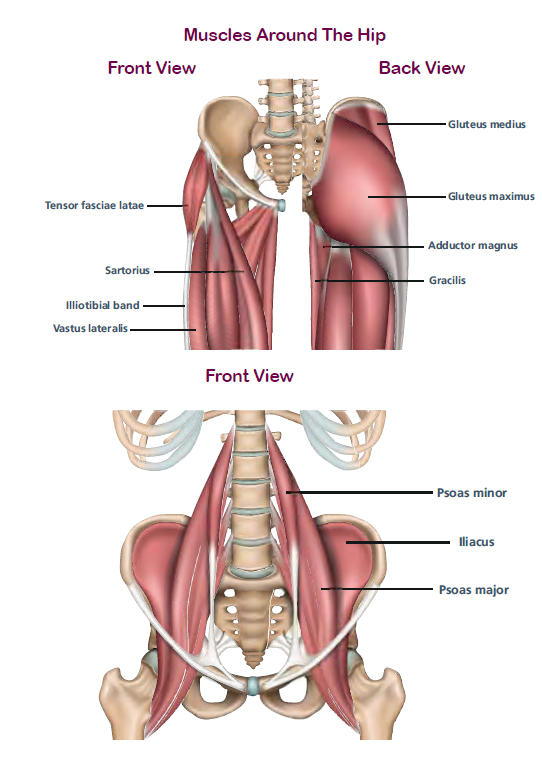
- Muscles: Strong muscles surround the hip joint, and need to work in the correct muscle pattern to absorb and dissipate forces and reducealtered shearing patterns. The stronger the muscles are, the better the hip joint is supported.
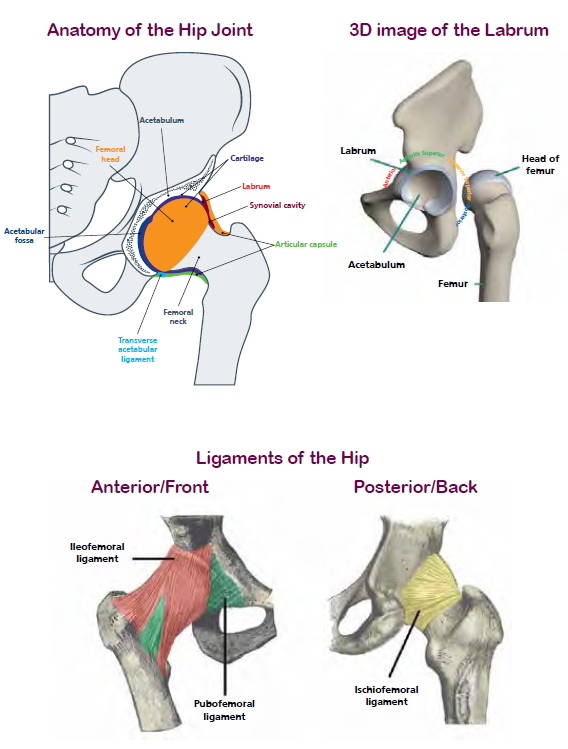
Labrum
The labrum is a horse-shoe shaped ring of cartilage which sits around the rim of the hip socket. It helps provide further stability and a suction seal. In a hip with dysplasia, there is increased movement of the ball in the socket due to lack of bone support, the labrum becomes thickened and inflamed to try and support the femoral head better. Eventually, it can become torn from taking the extra load. This is called a labral tear. The labrum has many nerve endings within it which can contribute to increased pain when it initially tears. However, studies show that up to 50% of people can have labral tears without any symptoms.
Hypermobility
Up to 50% of people with hip dysplasia can also have joint hypermobility. This means that joints have a greater range of movement than normal because the ligaments and joint capsule are lax (loose). This laxity means that the femoral head moves more within the socket and can also contribute to the uneven stress on the hip joint.
Summary
All the structures described contribute to making the hip stable. With hip dysplasia the hip joint is less stable because of the mis-shaped bones and also because often the ligaments and capsule around the joint can be lax (loose).
This lack of bony or ligamentous stability results in increased stress on the structures of the hip joint to try and contain the ball within the socket. There is increased shearing in the joint (there is a slightly greater amount of movement of the ball in the socket than in a normal hip joint).
If hip dysplasia is undiagnosed or untreated, the natural progression includes development of pain, functional limitations and then eventually degeneration of the joint, also known as Osteoarthritis (OA).
People with hip dysplasia can start to develop OA in their hip joint earlier than others because of the uneven wear to the joint. Think of a car tyre. If it is not aligned properly the tyre will wear down unevenly. The greater the degree of dysplasia and the prescence of subluxation the higher the risk of development of OA.
Symptoms
Those with Hip Dysplasia can experience a wide range of symptoms starting at any age. Normally patients present with pain after prolonged activity, and it is eased with rest. Most people experience pain in or around the hip or groin, but some report knee or back pain. Pain may be intermittent or more constant, it can come & go from day to day, or only occur with certain activities. Some symptoms you may experience include:
- Groin pain
- Pain deep inside the joint
- Pain at the front or side of your hip
- Pain when your hip is flexed to 90 degrees & turned inwards
- A limp or ‘waddling’ gait
- Clicking, catching or locking in the hip joint
- Feeling as if your hip will ‘give way’
- Pain that is made worse by activity & relieved with rest
- Some people experience knee pain, back pain or pelvic pain as well
Not everyone experiences all these symptoms, and you might experience different symptoms at different times.
Who has Hip Dysplasia?
If you find yourself with hip dysplasia as a young person or adult, you may have had a previous diagnosis as a baby. This is called Developmental Dysplasia of the Hip (DDH). It is sometimes known as ‘clicky-hips’ or ‘loose hips.’ You may have had treatment such as a pavlik harness or plaster cast or surgeries as an infant or child and have residual hip dysplasia now. However, you may not have had an infant diagnosis. Your symptoms might have started developing as a teenager or young adult after exercise or prolonged standing.
Why wasn’t it diagnosed when I was a baby?
The reasons why some cases of Hip Dysplasia are not picked up until later on young adult life are not fully known. One reason could be due to the fact that our current screening methods for Hip Dysplasia in infants don’t pick up every case. Another theory is that some forms of hip dysplasia develop during a growth spurt in adolescence and are linked to ligament laxity (hypermobility syndromes).
Why have I got it?
The causes of hip dysplasia still remain much debated and further research is required. However, there are some known risk factors that may play a part:
- First born
- Female gender
- Breech presentation
- Swaddling as a baby
- The heritable component of DDH due to common genetic links is approximately 55%. (links with GDF5 gene)
- Ligament laxity or hypermobility syndromes, or a family history of this - 47% more prevalent in DDH
Why has diagnosis taken so long?
It is not uncommon for people to find it takes a long time to find a clear diagnosis of hip dysplasia, the average time to diagnosis is 5 years. (Nunley et al, 2011).
Dysplasia often masquerades as other issues such as tight muscles and there are no specific clinical tests that diagnose dysplasia. You may have found you have seen a medical professional or Physiotherapist who has treated these other issues initially but that it has not helped your symptoms. It is important that you see a Physiotherapist and Consultant who specialises in dysplasia.
How is Hip Dysplasia Diagnosed?
Plain X-ray is the primary imaging technique used for diagnosis of hip dysplasia. An X-ray shows the bony anatomy, it does not look at soft tissue issues.
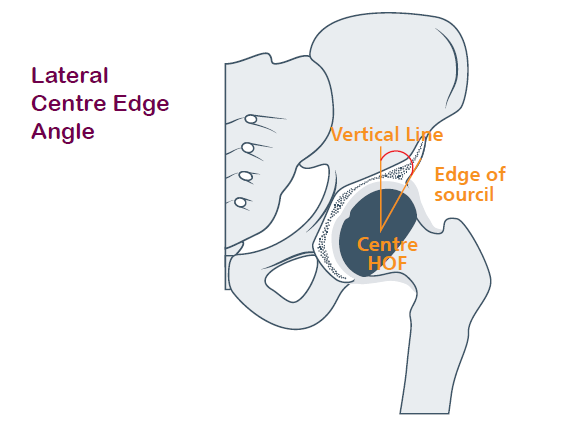
Important x-ray measurements include:
- The lateral centre-edge (LCE) - LCE angle is the most important angle to measure the lateral coverage of the socket over the femoral head, it measures from the centre of the head of femur (HOF) to the edge of the socket.
- An LCE of 18-25 is defined as mild or borderling dysplasia.
- An LCE of less than 18 degrees is defined as significant dysplasia.
Did you know?
‘Young adult hip’ refers to a speciality of orthopaedics dealing with hip problems in people from adolescence until roughly age 50. It separates it from elderly hip conditions.
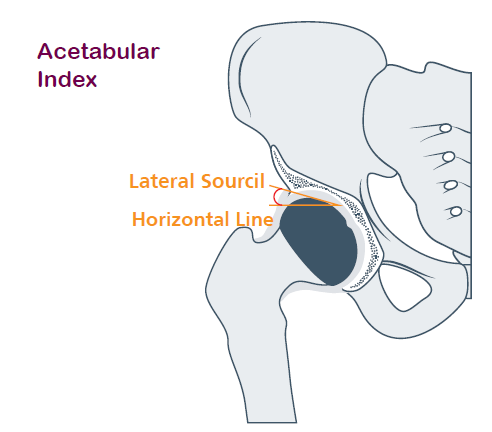
Acetabular Index
Sometimes called the sourcil angle This looks at the angle of the weightbearing zone of the socket, if the socket slopes upwards the joint will be less stable. In normal hips this is usually 7 – 10 degrees. In dysplastic hips this is over 10 degrees.
There are many other x-ray measurements which may be used to help in the diagnosis of hip dysplasia, but the main ones are the ones here:
- Alpha Angle - Indicates femoral head roundness.
- Shentons line - Indicates if the ball is sitting within the socket or not.
- Crossover sign - Indicates if the socket is orientated backwards.
- Anterior centre-edge angle - Measures coverage over the front of the socket.
- FEAR index - Predicts stability of the joint.
- Tonnis grade - Detects how much osteoarthritis is present
Other imaging investigations
MRI scan
A scan that takes pictures of your pelvis, to show the bone, cartilage, ligament, tendon and labrum in more detail. MRI scans are often used to assess the condition of the joint and to help decide on treatment options.
MRI Arthrogram
Dye or contrast is injected into the joint and then an MRI scan performed - this helps to highlight where contrast is leaking from the joint- indicating a labral tear.
CT Scan
Provides a 3D image reconstruction of the bone anatomy which will help diagnose complex multidirectional deformity and aid with surgical planning.
Arthroscopy
Also called ‘Keyhole surgery.’ The surgeon looks inside the joint to help diagnose your hip problem. In some cases it can be used to treat certain hip problems too.
It is recommended that you are seen by a specialist in Young Adult Hip conditions, as they are usually best placed to accurately diagnose your hip problem, rather than a general orthopaedic doctor.
Borderline Hip Dysplasia
Not all health professionals agree on what counts as Borderline Dysplasia.
However, most experts state it as having a centre-edge angle between 18-25 degrees. However, the 3-dimensional shape of the hip joint needs to be taken into account as well, so it is sometimes necessary to x-ray from both the front (AP view) and the side (called a ‘False profile’).
There is starting to be growing research into whether surgery (Periacetabular Osteotomy or Arthroscopy) or conservative treatment is best for borderline dysplasia, and there may be factors which can influence this. Activity levels, lifestyle, body weight, muscle strength, movement patterns and symptoms can all play a significant part.
Did you know?
Hip Dysplasia is a spectrum of conditions of the hip socket, from very mild or borderline dysplasia, through to severe dysplasia or even a partially dislocating hip joint. Remember everyone is different. We all have different shaped bones and there is no one perfectly shaped hip.
Related Hip Conditions
Acetabular version
Acetabular Retroversion
A normal hip socket is like an upside-down cereal bowl tilting slightly forwards. Acetabular Retroversion is like an upside-down bowl which is tilting backwards so the shallow part of the hip socket occurs at the back. It is usually measured on x-ray by using the
‘cross-over sign.’ This shows a faint line behind the femoral head denoting where the back part of the hip socket is too shallow. Those with acetabular retroversion may have similar signs and symptoms to those with hip dysplasia, however, they may also have trouble sitting or squatting & may experience pain at the front or back of the hip when attempting these movements.
Acetabular Anteversion
In contrast acetabular anteversion occurs when the socket is turned too far forwards and you get anterior uncovering of the femoral head.
Hypoplasia
Not Enouch acetabulum - Sourcil (roof of acetabulum) horizontal but short. This means you get lateral uncovering of the femoral head and antero-lateral instability.
Femoral Anteversion/Retroversion
Just like the socket, the femoral head (ball) can also be rotated forwards (anteversion) or backwards (retroversion). With femoral anteversion you may notice that you walk with your toes turned in. With retroversion you may notice that you walk more with your toes turned out, this is to naturally align your hip joint better.
Some patients may have a combination of both dysplasia and versional abnormalities, which affect the overall coverage of the hip and contribute to instability.
Femoro-Acetabular Impingement (FAI)
Femoro-Acetabular Impingement (FAI) also known as Hip Impingement, is a condition in which there is excessive bone growth on the edge of the femoral head (Cam lesion) or on the edge of the hip socket, causing overhang (Pincer).
Cam impingement results in a bump which may pinch on the hip socket during certain movements, and this bump (altered shape of the ball) can be present along with dysplasia. Pincer Impingement is unlikely in the presence of dysplasia (Wyatt et al, 2017).
Those with FAI can experience similar symptoms to those with Hip Dysplasia, but it is less certain whether all types of FAI will lead to early hip arthritis in the same way as Hip Dysplasia.
Treatment options
You will generally have 2 main options for treating hip dysplasia: nonsurgical (known as “conservative” treatment) such as physiotherapy, modifying your lifestyle and pain management, or surgical treatment to correct the shape of the hip socket itself. Surgical treatment to prevent OA developing in the hip joint is known as ‘Hip Preservation Surgery’.
Conservative Treatment Options
Physiotherapy
Physiotherapy is a key conservative measure which can help improve your symptoms. Patients often present with poor posture, muscle weakness, poor joint position sense, and associated secondary issues such as gluteal or psoas tendinopathy.
Physiotherapy should focus on:
- Improving posture, core strength and pelvic position awareness.
- Gait re-education - reducing stride length and preventing over extension of the hip.
- Optimizing lower limb muscle strength, especially hip extensors and hip rotators.
- Joint and body awareness exercises (Proprioceptive training).
- Education on nutrition, physical activity and self-management advice.
- Pain-management techniques - understanding how pain works and how to manage it with pacing and relaxation.
Whether you decide to have surgery or not, physiotherapy will play a significant part of helping with your hip problems. Physios are specialist at diagnosing and treating joint & muscle problems to reduce pain. You will benefit from finding a physiotherapist experienced in treating young adult hip issues and hip dysplasia patients.
Pain medication
Painkillers (e.g. paracetamol) and anti-inflammatories (e.g. Ibruprofen, naproxen) are all pain-relieving drugs. Speak to your GP about what medication it is best for you to take.
Modifying your lifestyle
You may find that modifying your lifestyle helps you manage your hips on a day-to-day basis, in the following ways:
- Maintaining a healthy weight
- Nutrition/dietician input
- Stopping smoking - smoking significantly affects bone healing if you are considering surgery- this is vital
- Staying active with low-impact exercise such as swimming (frontcrawl) or cycling. Breastroke can sometime irritate pain but everyone is different
- Making adjustments at work
Injections into the hip joint
Hip injections into the joint using local anaesthetic and Corticosteroid (high dose anti-inflammatory) are often used as both a diagnostic tool and a pain-relieving method. If the injection into the joint helps, this is a reliable indicator that the pain is coming from within the joint itself. Injections also help to break the pain cycle so Physiotherapy can commence. (Byrd and Jones, 2004).
Unsure what to do?
Sometimes watching and waiting and optimizing your conservative management strategy can allow information about your diagnosis to sink in and give you time to work out how best to manage your hip pain. Undergoing surgery is a big decision & it will be important for you to discuss with friends & family how employment, childcare & other arrangements would work if you do decide to go ahead with it.
Surgical treatment options
The focus of Surgical treatment is to restore stability of the hip joint by correcting the structural deformity either on the femoral or acetabular side.
Rarely in mild dysplasia an arthroscopy as an interim procedure may help relieve symptoms but will not address the underlying structural abnormality.
The aim of surgery is to provide more optimal coverage of the femoral head, this therefore reduces the shearing forces acting on the joint- reducing pain and delaying the progression to osteoarthritis (OA) (Albinana et al, 2004).
The gold standard hip preserving procedure for the treatment of hip dysplasia before the onset of osteoarthritis is a Pelvic osteotomy or Peri-Acetabular Osteotomy (PAO).
Good surgical outcomes depend upon the right patients being operated on in a timely manner. Factors that have been highlighted to significantly increase risk in poor surgical outcomes include: High BMI, Aged >40, Evidence of osteoarthritic changes of the joint (once the joint has started to fail the benefits of a PAO are limited). Previous surgery length and length and steepness of sourcil.
Pelvic Osteotomy or Peri-Acetabular Osteotomy (PAO)
A pelvic osteotomy is considered in patients who demonstrate symptomatic acetabular dysplasia with minimal signs of joint degeneration (Tonnis grade 0-1). A pelvic osteotomy in joints with significant joint degeneration is contraindicated and would soon require conversion to a total hip replacement (Clohisy et al, 2009).
It is extensive surgery which requires making three cuts in three different areas of the pelvis in order to free the hip socket, this then allows reorientation of the socket in any plane (direction) required to optimise the coverage over the femoral head. Screws are then used to hold the bones in the correct place whilst they are healing. There are 2 main types of Pelvic Osteotomy used in young adults:
- PAO also known as Ganz Osteotomy or Bernese Osteotomy
- Triple Pelvic Osteotomy (TPO) (a modification of which is known as the Birmingham Interlocking Pelvic Osteotomy (BIPO)
These are different techniques used to perform the surgery, but the idea is the same. They have both been shown to delay the onset of OA in the joint. Whilst a Pelvic Osteotomy is major surgery there is a relatively low complication rate. It will take approximately 1 year to rehabilitate postoperatively and Physiotherapy is key to the outcome and success of surgery.
You will need somebody to act as a main carer to begin with and having a support network can be really helpful. You will be shown exercises to do by your Physiotherapist and it’s really important that you persevere with these to regain joint movement and correct muscle patterning and strength, and achieve functional goals.
The operation can delay the need for a total hip replacement for up to 20 years in the vast majority of patients and yield excellent results and pain relief (Matheney et al, 2010). A small percentage will need a total hip replacement.
You will be flat foot touch weight-bearing up to 20kg (Weight bearing status may differ between surgeons and type of pelvic osteotomy) on crutches for 6-12 weeks. If you have a desk based job you can return when you are ready any time after 2-4 weeks but if you have an active job it is likely to be 3-4 months with a phased return required. Driving is usually allowed once you are full weight bearing and can perform an emergency stop.
Arthroscopy
This is also called keyhole surgery and involves using a tiny camera to look inside the joint. It can be used to help diagnose & treat some hip problems, for example, treating a labral tear. Arthroscopy can sometimes be used in cases of mild/borderline hip dysplasia, however, in most cases it is not indicated to treat a labral tear if hip dysplasia is the underlying cause of this, as the dysplasia itself needs to be corrected. This cannot be done using arthroscopy alone.
Femoral Osteotomy
If your femoral head is an altered shape or angle, a femoral osteotomy may also be performed alongside a pelvic osteotomy or on its own. This involves making a cut in the thigh bone (femur) and rotating it to a better position, and fixing with a plate and screws whilst it heals. This improves the alignment of the femur in the socket. Like with a pelvic osteotomy it involves being on crutches and physiotherapy rehab afterwards.
Total Hip Replacement (THR)
If you have significant osteoarthritis evident on your x-ray and MRI then a PAO is not indicated as it will fail to resolve the pain, and therefore the operation of choice is a total hip replacement. You may also require a hip replacement after having had a previous pelvic osteotomy in the past, and the joint has degenerated further.
A THR involves replacing the hip joint with an artificial one. Recovery from a THR is usually easier than from a PAO due to the surgical method, and weight-bearing status. Rehabilitation is still a vital component of recovery and can take up to a year.
Pregnancy, relationships & family life
Will having hip dysplasia affect me in pregnancy?
It is fine to get pregnant if you have hip dysplasia. Extra weight carried through pregnancy will increase the load going through the hip joints, which may increase your pain.
If you have hypermobility, your hip pain can increase during pregnancy as the hormone relaxin increases ligament laxity in preparation for the birth- this results in less stability from the ligaments around the hip joints and can cause increase shearing and therefore pain. Physiotherapy, maintaining strong muscles and pelvic corsets can help with this. If you have had a pelvic osteotomy, this surgery does not encroach the birth canal and therefore you can deliver normally if you wish.
Can I pass this onto my children?
Hip dysplasia is approximately 12 x more likely when there is family history. If you have a diagnosis of hip dysplasia it is important that your newborn child has an ultrasound screening. (International Hip Dysplasia Institute).
Can I still be intimate with my partner?
Being intimate with your partner is a key part of your relationship but your hip pain may make you worried or anxious about this.
The most important thing is to be honest with your partner about what is painful and uncomfortable. Positions that force the hips into extreme movement and full flexion may be more painful. Keeping your core stable, with your feet on something will provide improved joint position sense and reduce unstable feelings.
Seeking support
Receiving a diagnosis of hip dysplasia can be overwhelming. You might feel sad, angry, uncertain of the future or even relieved to find out what is wrong. All these feelings are normal. It’s important to know that you are not alone, there are many others with this condition, and seeking support (see final page for support groups), coping strategies & practical tips from others can be really beneficial, whatever treatment you decide on.
It can also take a while for information about your condition to sink in.You may want to keep this leaflet to refer back to. You can find details of online support networks & further resources on the back page. If you have chosen to undergo surgery then talking to others with hip dysplasia can help you feel prepared for what to expect and what recovery will be like.
One of the most important things in the journey of hip dysplasia diagnosis is acceptance of the diagnosis and then moving forwards.
Believe in what you can achieve, not in what you cannot do.Optimism is the faith that leads to achievement. Nothing can be done without hope and confidence.
The importance of Prehabilitation and Rehabilitation
Prehabilitation
You may have seen a Physiotherapist at some point through your journey to diagnose your hip pain, and you may have found that the treatment then, did not help your pain. This could be because you had a secondary issue (such as tendon pain) due to the dysplasia.
It is important once you receive the diagnosis of hip dysplasia that you see a Physiotherapist who specializes in DDH. Whilst the anatomy of the bones may be less than ideal and you might have hypermobility as well, think about all the other components of the joint that provide stability for the hip. If you can focus on improving this stability and reducing the loading forces, then this can really help with symptom relief.
Whether you decide to proceed with surgery or not, the stronger and fitter you are globally, the faster you will recover. Many patients report that the hip is too painful to rehab, the key fact is finding something that you can do and building from there, pacing yourself. Strengthening your core, adapting your posture and gait and improving your calf muscle strength can all significantly change the loading patterns on the anterior structures of the hip and therefore for example reduce the overload on the psoas tendon irritation as well as the labrum.
Can you manage with a labral tear?
Yes! In the acute phase the tear may be symptomatic and painful. But if you improve the proprioception (joint position sense) and reduce the amount of shearing on the front of the joint, then the tear can become asymptomatic. MRI studies have shown that up to 50% of people can have labral tears with no symptoms (Lee et al, 2015 and Tresch et al, 2017).
One of the most important things in the journey of hip dysplasia is acceptance of the diagnosis, and then formulating a plan to move forwards. Understanding how to move forwards is vital and building a team of people around you who can do that with you is key. Setting goals and action plans, help focus your rehabilitation.
A muscle strengthening programme is key, many patients have poor muscle patterning around the hip and weak muscles in other areas as well. To optimize loading of the hip joint for walking you need to have good single leg control and have strong enough muscles to propel your body weight forwards and upwards in order to take a step (remember how much our bodies weigh- EG 65KG your muscles need to be strong enough to push that weight on one leg). For example, if you struggle to stand on one leg and raise your heel off the floor repetitively, then you will swing through the anterior hip more to gain propulsion- therefore stressing the hip joint and labrum further- strengthen the calf, foot and gluteal muscles, and you reduce the forces on the anterior hip and reduce your pain.
Closed chain based exercises- (exercises with the foot on the floor) are also a key starting point in the rehabilitation of hip dysplasia- this is because it improves the joint position sense and recruitment of the correct muscles.
Rehabilitation - Post Surgery
Rehabilitation post-surgery is critical to the outcome of the surgery. Altered movement patterns and muscle timing occur due to pain pre-op and these movement patterns are maintained post operatively, it is vital to correct this and restore normal mechanics.
After pelvic osteotomy surgery you will be protected weight-bearing on the operated leg with crutches for roughly 6 – 8 weeks. Your surgeon will give you specific instructions of precautions and what movements should be avoided to begin with. It is important that you start physiotherapy early to restore movement, maintain joint range and start strengthening unloaded. If you have access to hydrotherapy, once the wound is healed it is also advantageous in the short term.
This period of unloading of the operated leg will affect all of the muscles in that leg and they will be significantly weak. Once the check x-ray is performed at 6-8 weeks (depending on your surgeon), and bony healing is confirmed on x-ray, you will be allowed to gradually increase the weight through your operated leg and commence a strengthening programme.
Remember it takes 6 weeks to see significant strength changes in muscle so recovery can take up to 1 year. The more focused you are on your rehabilitation the less likely you are to get secondary issues post-operatively (such as gluteal tendinopathy). (Hunt et al, 2012).
What does the future look like?
You may have decided what treatment you are having, or you may be unsure or still considering your options. Talk to your doctor, surgeon or healthcare practitioner about what is best for you. Don’t be afraid to ask questions about your future with Hip Dysplasia.
Some people find that after surgery they are still prone to fatiguing with physical activity and have to make work adjustments in the long run, especially with more physical job roles. Some find that they can return to impact sports, others find non-impact sports suit them better. Everyone is different and there are many factors which have an influence on people’s lives with Hip Dysplasia. There is a small but growing research base into Hip Dysplasia and our understanding of the condition is growing all the time.
It’s important to remember that treatment options for hip dysplasia are aimed at reducing pain and delaying the development of OA in the joint.
Therefore if you choose to undergo hip preservation surgery, you may still need to undergo THR at a much later time in your life. However, there is still a good possibility of going on to live a functional, pain-free life, and delaying a THR for many years.
For more information
International Hip Dysplasia Institute
An international charity committed to researching & raising awareness of hip dysplasia
www.hipdysplasia.org
I’m A Hippy
An international website/charity/patient and professional network regarding hip dysplasia.
www.imahippy.org
Steps Charity UK
A charity supporting children & adults affected by paediatric lower limb conditions
www.steps-charity.org.uk
DDH UK
A charity providing information & support for those affected by Hip Dysplasia
www.ddh-uk.org
‘Hip Dysplasia Physio- Information and support regarding Physiotherapy for Hip Dysplasia’
Hip Pain Help
www.hippainhelp.com/acetabular-dysplasia/